Treatments
Corneal transplant
What is corneal transplant?
Also called keratoplasty, corneal transplantation is the most widely performed type of transplantation in Spain. It consists of replacing the diseased or damaged cornea, due to alterations in its shape or transparency (essential features for us to be able to see clearly), with a healthy cornea from a donor.
There are multiple techniques we can perform, which are mainly grouped into:
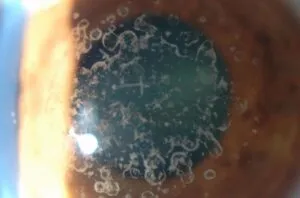
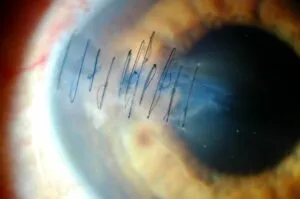
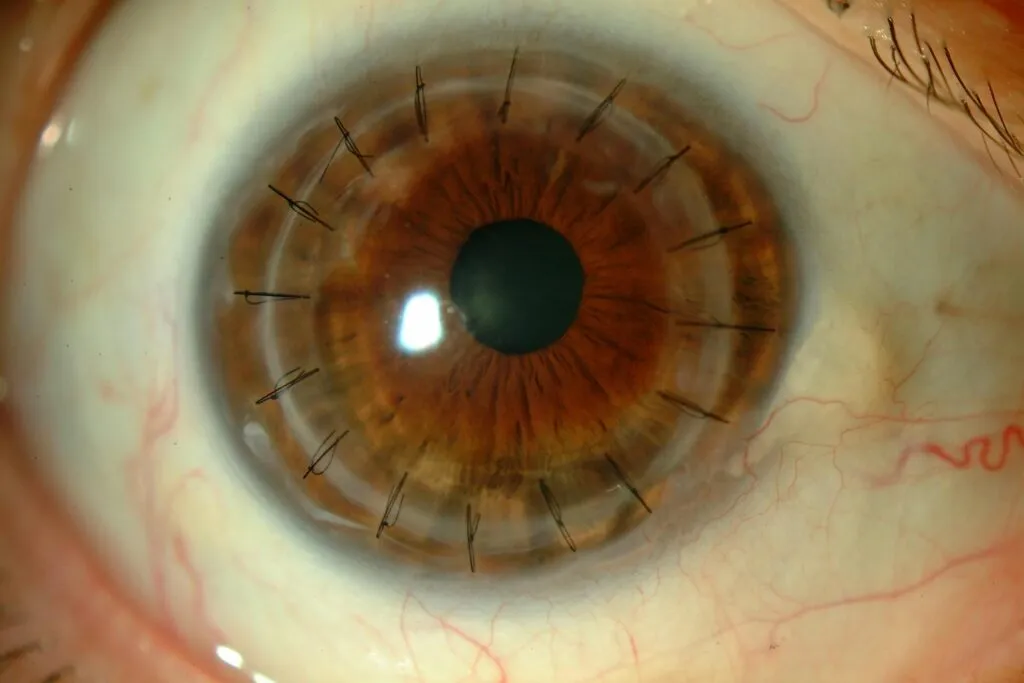
- Penetrating or complete corneal transplantation: we replace the entire cornea.
- Selective or partial lamellar corneal transplantation: we only replace the affected parts of the corneal tissue. We opt for anterior lamellar transplantation when the lesion is in the stroma (intermediate layer that covers approximately 90% of the total corneal thickness). Otherwise, if what is altered is the endothelium (layer that lines the inside of the cornea), we perform a posterior lamellar transplantation.
The cornea is barely half a millimetre thick, whereas the endothelium, for example, is so thin that it does not exceed 20 microns. Handling these delicate and complex eye structures requires great skill on the part of the ophthalmic surgeon, although selective keratoplasties are really the most convenient for the patient, when there is the possibility of performing them.
Thus, specialists at the Miranza clinics are pioneers in the application of this type of corneal transplantation, having performed the first surgeries in Spain and contributed to the development of minimally invasive techniques, such as DMEK (Descemet’s Membrane Endothelial Keratoplasty).
Eye diseases treated by cornea transplant
Furthermore, corneal transplantation may also be indicated in case of deep corneal infections or scars caused by these infections, as well as corneal oedemas after intraocular surgeries.
Recovery
This is an outpatient surgery, performed under local anaesthesia, which usually lasts between 40 and 60 minutes. The postoperative period is generally not painful (only slight discomfort) and the recovery period will vary depending on the technique applied.
For example, after a penetrating or total keratoplasty, you can return to your normal activity in 3-4 weeks, although the stitches remain in the eye for about a year, so your visual acuity will fluctuate until they are removed and the new cornea is accommodated. In contrast, with some anterior lamellar keratoplasty techniques, the stitches are removed after 6 to 8 weeks, while endothelial transplants such as DMEK even avoid the use of sutures and recovery is completed in just 4 to 6 weeks.
One of the advantages of selective corneal transplantations is that they speed up recovery, as well as offering a higher degree of final vision than a complete conventional transplantation, even reaching 90-100% of the patient’s potential vision.