Sleep apnea increases the risk of developing glaucoma
Sleep apnea can affect ocular circulation and promote the development of glaucoma. Therefore, preventive eye exams are recommended for patients with a family history or ocular hypertension.
Sleep apnea, a respiratory disorder that affects millions of people, may be closely related to the progression of glaucoma. Recent studies suggest that individuals with sleep apnea show a higher prevalence of glaucomatous damage. Glaucoma is a chronic disease of the optic nerve and one of the leading causes of irreversible blindness, which in many cases presents no symptoms until its advanced stages.
“Sleep apnea may contribute to the development and progression of glaucoma. It has been observed that snoring patients with apnea have a higher risk of developing glaucoma, especially the subtype known as normal-tension glaucoma or low eye pressure glaucoma, as well as a greater risk of experiencing worsening of the disease compared to those without sleep-related breathing disorders,” explains Dr. Fernando López, glaucoma specialist at Miranza Instituto Gómez-Ulla.
Intermittent hypoxia that occurs during nocturnal episodes, along with alterations in intracranial pressure and reduced blood flow to the optic nerve, are mechanisms that could contribute to the progressive deterioration of the visual field in patients with or without a prior diagnosis of glaucoma.
Control Sleep, Protect Vision
The connection between both disorders can be explained by several mechanisms: the repeated lack of oxygen each night and the blood pressure changes associated with apnea can alter blood circulation in the optic nerve and retina, which may contribute to the ocular damage characteristic of glaucoma. Recognizing this relationship has important clinical implications. Snoring patients with apnea could benefit from regular eye examinations to detect early signs of glaucoma and monitor disease progression. Similarly, those diagnosed with glaucoma could benefit from evaluation for sleep-related breathing disorders in order to address potential modifiable risk factors.
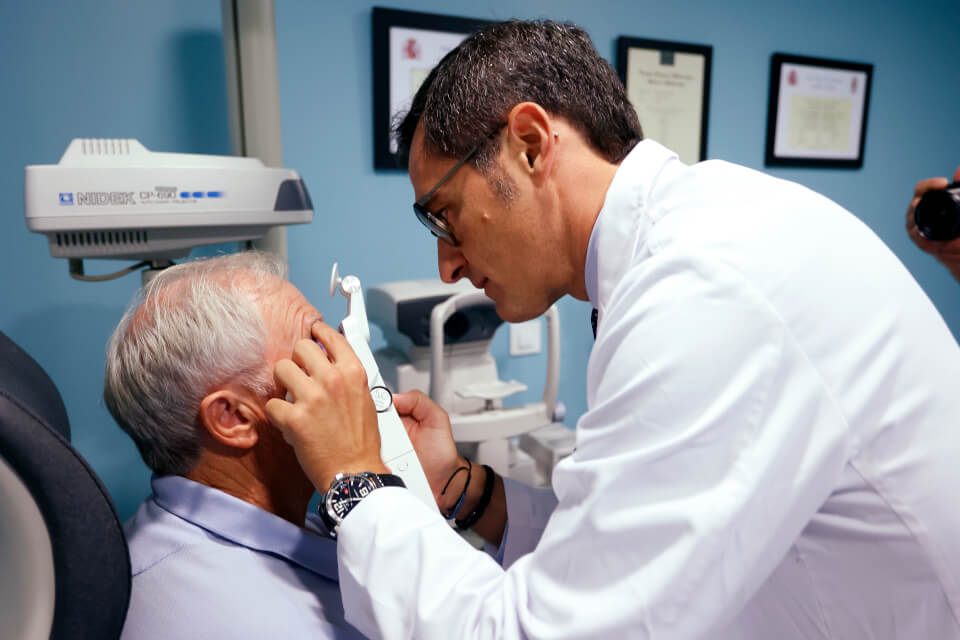
This is why emphasis is placed on the importance of multidisciplinary care that integrates ophthalmological evaluation into the follow-up protocols for patients with apnea. “It is not only about controlling sleep, but also about protecting vision. Many of these patients show no visual symptoms until the damage is irreversible,” says Dr. López, stressing the importance of conducting preventive eye exams in patients diagnosed with sleep apnea, especially if there is a family history of glaucoma or ocular hypertension.